PELVIC ORGAN PROLAPSE
Home / Services / Gynaecology / Pelvic organ Prolapse
Pelvic Organ Prolapse
The pelvic organs include the bladder, uterus and cervix, vagina, and rectum are all supported by the pelvic floor muscles like a hammock. When these pelvis muscles and tissues can no longer support these organs prolapse occurs.
Pelvic organ prolapse (POP) appears like a lump in vagina and may cause symptoms such as heavy, dragging feeling or lump in the vagina, bladder or bowel problems and discomfort with sexual intercourse. Many women are embarrassed to see their doctor with this issue .It is not uncommon and is seen in 50% of women above 50 with some degree of POP.
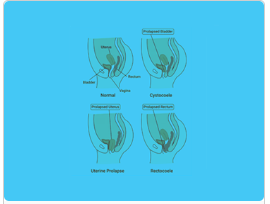
Different types of POP include :
- Cystocele (Bladder wall prolapse) . This is the most common type of pelvic organ prolapse. This happens when the bladder drops into or out of the vagina.
- Rectocele. This happens when the rectum bulges into or out of the vagina.
- Uterine Prolapse : This happens when the entire uterus bulges into or out of the vagina and may be sometimes associated with small bowel prolapse into the vagina. Rarely, pelvic organ prolapse can also happen after a hysterectomy. Any part of the vaginal wall may drop, causing a bulge into or out of the vagina.
Risk factors for POP include:
- Prolonged and difficult vaginal child birth -damage to pelvic floor muscles and tissues.
- Smoker and or Chronic cough
- Age & Menopause – lack of Estrogen after menopause also cause tissues to become slack and may contribute to POP.
- Chronic constipation
- Family history
Symptoms include
- Feeling or seeing a bulge in the vagina or outside.
- Pressure discomfort and aching in pelvis and thighs.
- Leaking urine (incontinence)or leaking stool.
- Problems inserting tampons.
How is POP diagnosed?
A detailed medical history and vaginal examination including a speculum examination to assess and measure the stage of prolapse.Coughing while examination helps to assess if urinary leakage is a problem.
If you have any bladder symptoms, we may recommend special bladder studies, known as a urodynamic assessment, to help diagnose the cause and determine the best treatment options for you.
How is pelvic organ prolapse treated?
Treatment depends on the type of prolapse you have, your symptoms, your age, other health problems, and whether you are sexually active.
- Pessary: A pessary is a plastic or silicone removable device inserted into the vagina to support the pelvic organs. They come in different sizes and may be the first choice of treatment or if the patient is not fit for surgery.
- Pelvic floor exercise: Pelvic floor muscle exercises Kegels exercises can also help women who have mild to moderate prolapse and also helps in women with urinary incontinence.
- Life style modifications: Losing weight, quit smoking, avoiding constipation, avoiding heavy weight lifting and strenuous abdominal exercises.
- Surgery: Depending on the type of prolapse and symptoms you may want to consider surgery if other options have not adequately helped. Surgery for POP aims to support the pelvic organs and restore them to their natural position and to help ease your symptoms. Surgery for prolapse can be performed either through the vagina or through the abdomen.
- Vaginal approach: To repair the cystocole, rectoceole, and sometimes vaginal hysterectomy is recommended.
Surgery to close the vagina. This surgery, called colpocleisis, treats prolapse by closing the vaginal opening. This can be a good option for women who do not plan to have or who no longer have vaginal intercourse.
Is mesh safe to use during surgery to repair pelvic organ prolapse?
Mesh used to repair pelvic organ prolapse through the abdomen is safe. But, because of safety issues, mesh is no longer used to repair prolapse through the vagina.If you had surgery with mesh to repair pelvic organ prolapse through the vagina, you may not need to do anything if you do not have any symptoms or problems. Talk to your doctor or nurse if you notice any symptoms or problems, such as vaginal bleeding or discharge, pelvic pain, or pain during sex.
